Surgical Procedures Commonly Performed
Head Non-Surgical Care and Management
Head Surgical Care and Management

Aneurysm Clipping
Bifrontal Craniotomy for Tumor
Brain AVM Resection (Cerebral Arteriovenous Malformation Resection)
Burr Hole Drainage
Craniectomy for Chiari Malformation (Foramen Magnum Decompression)
Cranioplasty
Craniotomy for Epidural Hematoma
Craniotomy for Intracerebral Hematoma
Craniotomy for Meningioma (Brain Tumor)
Craniotomy for Subdural Hematoma
Craniotomy for Tumor
Deep Brain Stimulation (DBS)
Deep Brain Stimulation (DBS), Frameless Method
Embolization for Cerebral Arteriovenous Malformation (AVM)
Microvascular Decompression for Trigeminal Neuralgia
Ommaya Reservoir Placement
Pituitary Tumor Surgery (Transsphenoidal Approach)
Stereotactic Brain Biopsy (Needle Biopsy Method)
Stereotactic Radiosurgery for Arteriovenous Malformation (AVM)
Suboccipital Craniectomy for Acoustic Neuroma
Ventriculoperitoneal Shunt for Hydrocephalus
Peripheral Surgical Care and Management
Spine Surgical Care and Management
ALIF: Anterior Lumbar Interbody Fusion
ALIF: Anterior Lumbar Interbody Fusion (with bone graft and metal plate)
ALIF: Anterior Lumbar Interbody Fusion (with bone graft and pedicle screws)
Anterior Cervical Corpectomy
Anterior Cervical Discectomy and Fusion (ACDF)
Anterior Cervical Discectomy and Fusion, with Cage
Artificial Cervical Disc Replacement (Mobi-C®)
Cervical Laminaplasty (Cervical Laminoplasty)
Cervical Posterior Foraminotomy
Laminectomy
Laminectomy (Cervical Spine, With Fusion)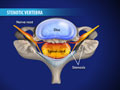
Laminectomy (Cervical)
Lumbar Corpectomy
Lumbar Disc Microsurgery
Lumbar Interbody Fusion (IBF; LIF)
Minimally-Invasive Lumbar Microdecompression
Minimally-Invasive TLIF (Transforaminal Lumbar Interbody Fusion)
Posterior Lumbar Interbody Fusion (PLIF)
Spinal Fusion (Lumbar)
TLIF: Transforaminal Lumbar Interbody Fusion
XLIF® Lateral Lumbar Interbody Fusion